By Maya Morris
Images courtesy of Cardiovascular Institute of Scottsdale
When patients have atrial fibrillation — a medical term for an irregular heartbeat — they have a five times higher risk for stroke than the average population. Since the 1950’s, the accepted treatment for AFIB has been Warfarin, a blood thinner doubling as a rat poison. Now, Eliquis or Xarelto are offered in place of Warfarin.
However, any blood thinner comes with the same risk. “Every year that they don’t have a major bleeding event, their risk for a major bleeding event goes up,” Kim Krmpotic, a nurse practitioner specialized in electrophysiology, added. She works alongside Dr. Sadhu both in the clinic and in the hospital. Once someone begins taking blood thinners, she said, they take it for a lifetime.
Common operations for AFIB involve radio frequency therapy or cryoablation therapy. This thermal approach comes with its own set of risks. When heat or freezing is applied to the inside of the heart, to treat the irregular heartbeat, there is a possibility of damaging the esophagus behind it. Now, however, a safer ablation method has been introduced.
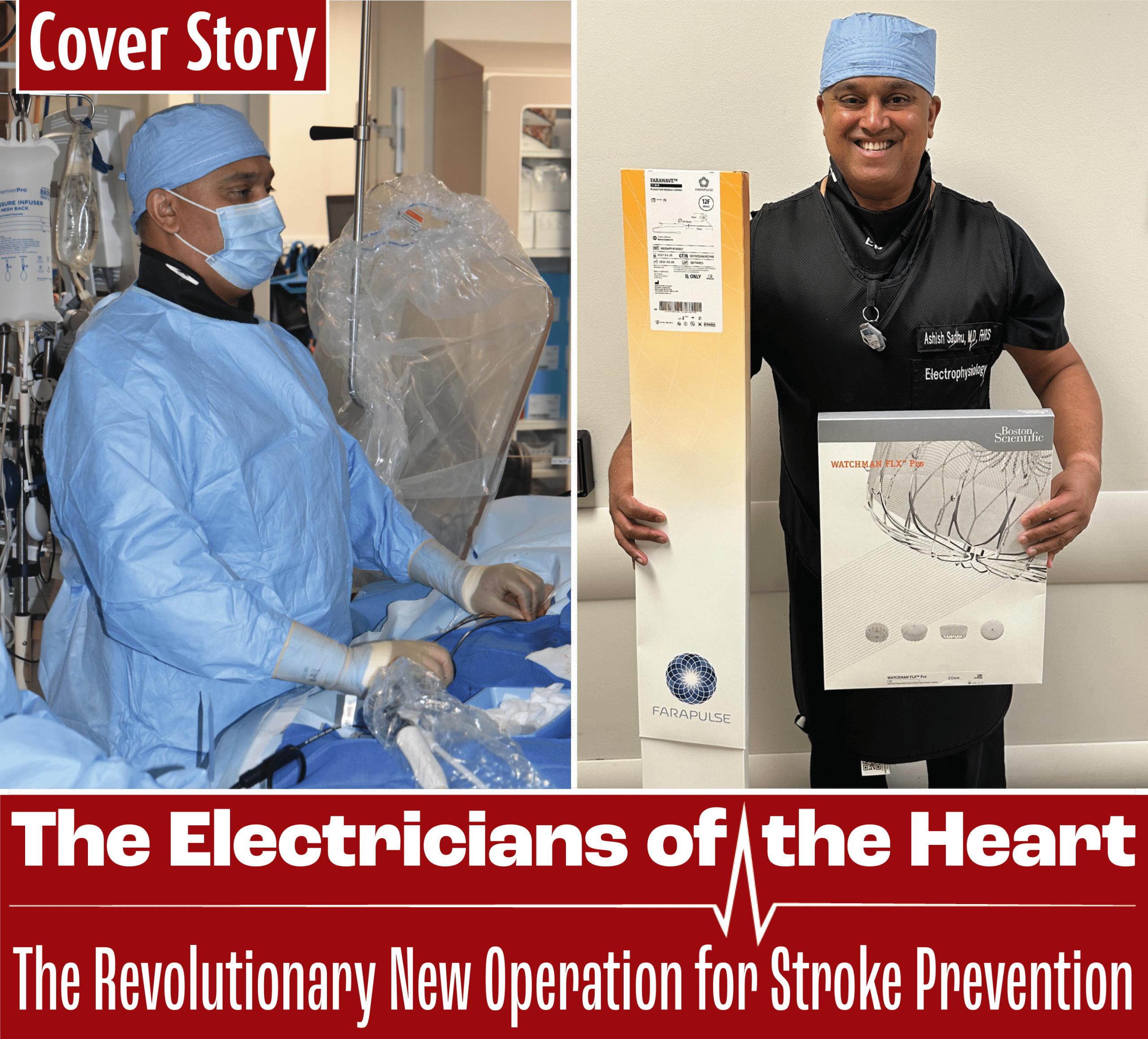
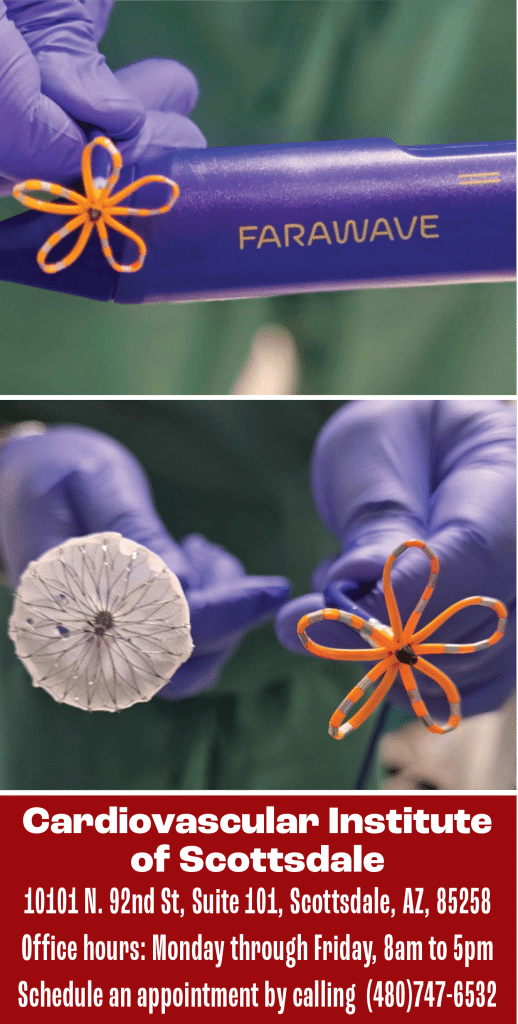
The Farapulse PFA system greatly reduces the risk of damaging the heart by using nonthermal energy. It sends direct pulses of electric energy into the areas which cause the irregular heartbeat. This procedure offers a safer alternative, especially for seniors, and expands the range of patients that can be treated.
After any ablation therapy, however, the patient must remain on blood thinners.
“What if we can offer you a procedure that can work on your rhythm control…and implant WATCHMAN for getting you off the blood thinners?”
Dr. Sadhu can do just that. He was one of the first to do a concomitant procedure which was approved in October 2024, and to implement Boston Scientific’s WATCHMAN device — a small, round object that blocks the left atrial appendage within the heart. The LAA is shaped in the form of a pocket, which can collect blood clots and cause a stroke. By closing this appendage with the device, it minimizes the chances of suffering a stroke and eliminating the need for long term blood thinners.
Patients must be high on the CHADSVASC score — a system that ranks how high the stroke risk is — to qualify for the procedure.
Dr. Sadhu performs a concomitant procedure, which combines both the Farapulse Ablation and WATCHMAN device. While the Farapulse system treats the irregular heartbeat, the WATCHMAN simultaneously treats the stroke risk. The WATCHMAN is inserted through an incision near the groin and is implanted into the LAA. After it is implanted firmly into the heart, and successfully passes a criteria, the patient could go home the very same day.
While every procedure has risks, the WATCHMAN’s are significantly low. The latest device has a HEMOCOAT technology that promotes healing, so a layer of skin can grow over it and safely block the LAA. It also helps prevent blood clots from forming over it.
When someone has “palpitations, they feel their heart skipping or racing, they’re short of breath out of the ordinary to their normal day to day activities, they feel that they’re sleepy all the time,” Dr. Sadhu suggests they seek out medical attention, whether that be their primary care physician, the emergency department, or a cardiologist.
Deciding to proceed with an ablation or WATCHMAN is a big step. Kim Krmpotic highly encourages patients to talk it over with their families first.
The first consultation with Dr. Sadhu or his nurse practitioner takes about an hour to talk about patient history, goals, and potential treatments. Each case is different and requires a thorough investigation before any procedure can be considered.