By Lin Sue Flood
ALS has changed John Rosso’s life, but not in the way one might imagine. This cheery-natured Scottsdale resident doesn’t focus on what he can no longer do. Instead, the 73-year-old channels his energy into pushing boundaries and overcoming challenges posed by the neurodegenerative disease.
As his condition progressed and it became more difficult to speak, Rosso utilized “voice banking” to create a synthesized version of his natural speaking voice. A high-tech device uses those recordings to help Rosso vocalize his wants and needs to family, friends and his Hospice of the Valley care team.
“It’s a joy to see how John continues to thrive as he adapts to changes in his health,” says respiratory therapist Gretchen Stanton. “Machines like this add so much to his quality of life.”
The Eye Gaze PRC has eye-tracking cameras that read whatever phrase Rosso looks at on the screen. Then he clicks a joystick to “speak it out loud.” Speech language pathologist Jeremy Legaspi says the machine even allows people to type sentences by focusing their eyes on one letter at a time.
“John can take control of the computer, go online and interact with the world. Or he can just say whatever he pleases — like tell the dog to stop barking. It’s the difference between not being able to communicate with your family and being able to tell them I love you,” Legaspi says.
Other machines help compensate for the muscle weakness caused by ALS (amyotrophic lateral sclerosis), which makes it harder for Rosso to cough and clear his lungs. To help keep his airway clear, his hospice team has taught him to use a special respiratory cough assist device and suction machine.
“Think of it as a big air blower and vacuum,” explains Stanton. “The machine first pushes air into his lungs to inflate them, then powerfully sucks that air out along with any mucus. Then the suction wand can remove it and keep his airway nice and open.”
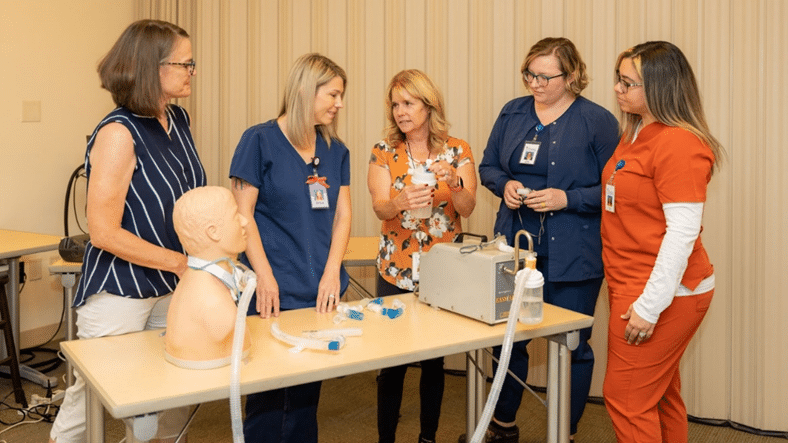
Hospice of the Valley’s unique Pulmonary Resource Program supports patients with neuromuscular diseases, emphysema, pulmonary fibrosis, lung cancer, COPD, and other conditions that affect breathing. Stanton and pulmonary nurse Barbara Taylor instruct clinical teams and family caregivers in using and monitoring respiratory equipment in the home.
“This is critical because our patients’ conditions can change very quickly,” says Hospice of the Valley physician Shelly Myers. “Settings on pulmonary equipment are adjusted as needed.”
Rosso’s wife, Kimberly, is grateful for the 24/7 support. “The whole team is a godsend and we don’t know what we’d do without them,” she says. “They are always just a phone call away and their special talent and knowledge provide a huge level of comfort for me.”
Taylor beams when talking about technology. “It’s a win-win when we can provide patients and families with exactly the right equipment and then customize it to keep them comfortable and safe.”
To learn more about Hospice of the Valley’s Pulmonary Resource Team, visit: hov.org/our-care/pulmonary-care